Review
Psychological
treatment approaches for improvement of maladaptive eating behaviors in
bariatric surgery patients: A systematic review
Tratamientos
psicológicos para el mejoramiento de las conductas alimentarias desadaptativas
en pacientes de cirugía bariátrica: revisión sistemática
Patricia
Ruiz-Cota1, Montserrat Bacardí-Gascón1, Carla I.
Fernández-Guerrero1, Arturo Jiménez-Cruz1
1
School of Medicine and Psychology, Autonomous University of Baja California,
Tijuana 22390, Mexico.
*
Corresponding Author.
|

This work is
licensed under a Creative
Commons
Attribution-NonCommercial-ShareAlike 4.0 International License
La
revista no cobra tasas por el envío de trabajos,
|
|
Abstract
Introduction. Maladaptive
eating behaviors (MEB) are highly prevalent among bariatric surgery patients
and have been demonstrated to be important contributors for weight loss
outcomes. A systematic review was conducted to evaluate the effectiveness of psychological
treatment approaches on MEB in bariatric surgery patients.
Materials and Methods. This systematic review was registered in PROSPERO. Literature review was
performed in the databases PubMed, ScienceDirect, Cochrane Library, and Web of
Science. We included studies published
between January 1st 1990 and October 18th 2019, with pre-
or postoperative psychological treatment
approaches in bariatric surgery patients
aimed to improve MEB.
Results. A total of
15 studies met the inclusion criteria (eight RCT and seven pretest-posttest
studies), 752 participants were identified, 80.3% were female and the average
participant’s age was 46.1 years (SD ± 6.6). Follow-up period after
intervention ranged from six weeks to 48 months. Five out of eight RCT reported
a positive and significant effect (P <0.05) on MEB and four had
medium to large effect size between the groups receiving psychotherapeutic
interventions and the control group. Six out of seven pretest-posttest studies
reported significant difference (P <0.05) on MEB and had small to
large effect size after receiving psychotherapeutic interventions.
Conclusion. Overall, the quality of the evidence ranged from low to
moderate. Psychological treatments in bariatric surgery patients are inconsistent,
though most results indicate improvement on MEB. Well-designed long-term
studies and other approaches strategies are warranted to assess the long-term
effects on MEB and weight loss in bariatric surgery patients.
Keywords
Maladaptive eating behaviors;
Psychological treatment; Psychotherapeutic; Bariatric surgery; Systematic
review
Resumen
Introducción. Las conductas alimentarias desadaptativas (CAD) son altamente
prevalecientes en los pacientes de cirugía bariátrica y han sido demostradas
ser contribuyentes importantes en los resultados de la pérdida de peso. Una
revisión sistemática fue realizada para evaluar la efectividad de los enfoques
de tratamientos psicológicos en CAD, en pacientes de cirugía bariátrica.
Materiales y métodos. Esta revisión sistemática fue registrada en PROSPERO. La revisión
de la literatura fue realizada en las bases de datos de PubMed, ScienceDirect,
Cochrane Library y Web of Science. Incluimos estudios publicados entre 1 de
enero de 1990 y 18 de octubre de 2019, con enfoques de tratamiento psicológico
pre o posoperatorio en pacientes de cirugía bariátrica destinados a mejorar las
CAD.
Resultados. Un total de 15 estudios reunieron los criterios de inclusión
(ocho ensayos clínicos aleatorizados (ECA) y y siete estudios
preprueba-postprueba),752 participantes fueron identificados, 80.3% fueron
mujeres y la edad promedio de los participantes fue de 46.1 años (DE ± 6.6). El
periodo de seguimiento después de la intervención varió de seis semanas a 48
meses. Cinco de ocho ECA informaron un efecto positivo significativo (P
<0.05) en las CAD y cuatro tuvieron un efecto de medio a alto entre los
grupos que recibieron intervenciones psicoterapeúticas y el grupo control. Seis
de los siete estudios preprueba-postprueba reportaron diferencias
significativas (P <0.05) en las CAD y tuvieron un tamaño de efecto de bajo a
alto después de recibir intervenciones psicoterapéuticas.
Conclusión. En suma, la calidad de la evidencia varió de baja a moderada. Los
tratamientos psicológicos en pacientes de cirugía bariátrica son
inconsistentes, aunque la mayoría de los resultados indican un mejoramiento en las
CAD. Estudios bien diseñados y otras estrategias de enfoque son garantizados
para para evaluar los efectos a largo plazo de las CAD y la pérdida de peso en
pacientes de cirugía bariátrica.
Palabras clave
Conductas alimentarias desadaptativas; Tratamiento psicológico;
Psicoterapia; Cirugía bariátrica; Revisión sistemática
Introduction
The prevalence of obesity has
risen in the past three decades, becoming a worldwide epidemic(1).
In 2016, according to the World Health Organization (WHO), over 650 million
adults (18 years and older) had obesity(2). Data from the National
Health and Nutrition Survey (NHANES) reported a prevalence of obesity among
United States (U.S.) adults of 39.8% in 2015-2016(3). Since the
1970s, obesity trends have been increasing in the U.S. regardless of ethnicity,
race, age, or gender(4).
Numerous interventions and
treatments have been developed to halt the progression of obesity. Metabolic
and bariatric surgery (MBS) has become one of the most commonly performed and
approved therapies for severe obesity(5,6). Substantial weight loss,
remission or improvement of related comorbidities have been widely demonstrated(7-12).
Recent research has proven a superior and persistent effect of MBS than medical
treatment in medium and long-term periods(13). However, despite the
outcomes regarding short- and medium-term weight loss after MBS, treatment
failures (≤50% excess weight loss)(14,15) can reach up to 5-20% in gastric bypass and gastric sleeve(16,17),
and 14-63% in gastric band(18).
Several non-surgical factors
have been identified to be associated with poor weight loss outcomes, weight
regain, and weight loss maintenance over time. Associated factors include a
variety of demographic, patient-related diseases, and behavioral
characteristics, from which older age, greater preoperative weight,
obesity-related diseases, physical inactivity, poor follow-up after surgery,
self-efficacy, psychosocial and behavioral patterns have been demonstrated to
play an important role(19-22). Maladaptive eating behaviors (MEB)
are highly prevalent among bariatric surgery patients and have been reported to
be much higher compared to the general population(23). The most
common MEB reported in the literature are binge eating, emotional eating,
uncontrolled eating, eating in absence of hunger, recurrent episodes of
nocturnal eating, and continuous snaking or grazing patterns(24).
These problematic eating patterns have been demonstrated to be significant predictors of poor weight outcomes(25).
MEB are associated with an increased caloric
intake, which causes less weight loss, weight regain, and attenuated long-term
weight loss can ultimately cause treatment failure(24,26-28). The
association between preoperative MEB and weight loss outcomes after surgery
have yielded inconsistent results, while there is consistent evidence of
postoperative MEB negatively affect weight loss results(29).
However, in the last years, research has been increasing evaluating the impact
that have preoperative MEB, specially binge eating, on postoperative outcomes.
A recent study reported that patients that presented higher levels of
pre-operative emotional eating and food addiction symptoms had poorer weight
loss 1 year after follow-up(30). In addition, other psychological
factors (depression, anxiety and drug abuse) are also associated with weight
loss outcomes and adherence to surgical protocols(31).
Behavioral interventions
including psychotherapy have been implemented in bariatric surgery patients
before and/or after surgical treatment to improve MEB, better compliance to
dietary guidelines, weight maintenance, and to optimize weight loss after
surgery. Psychological interventions are characterized by a large variety of
therapies, ranging from individual and group therapy to support groups(32).
Previous systematic reviews which evaluated behavioral management including
psychotherapeutic interventions and support groups in bariatric surgery
patients have demonstrated a positive effect on weight loss outcomes(32-34).
Most of the psychological treatment approaches developed for improvement of MEB
implement or are based on principles of cognitive behavioral therapy (CBT), acceptance-commitment therapy, mindfulness, adapted
motivational interviewing, and psychoeducational groups. These therapeutic
strategies provide skills to regulate eating patterns, stimulate self-control,
create assertiveness/problem-solving skills, increase self-esteem and
motivation to change(35,36).
The aim of this systematic
review is to evaluate the effectiveness of pre- or postoperative psychological
treatment approaches on MEB in bariatric surgery patients.
Methods
Protocol and Registration
The protocol of the present
study was registered at the international database of prospectively registered
systematic reviews in health and social care (PROSPERO), the registration
number is CRD42018108443.
Literature search strategy
The present study was
conducted in accordance with the Preferred Reporting Items for Systematic
Review and Meta-analysis (PRISMA) recommendations(37). A
comprehensive literature review was performed in the databases MEDLINE
(PubMed), ScienceDirect, Cochrane Library, and Web of Science. Additionally, we
performed a manual review of the reference list of retrieved articles for any
other related study not included in our database search. Literature search was limited to include studies between
January 1st 1990 and October 18th 2019. The following combinations of search terms were used:
“psychotherapy” OR “psychotherapeutic” OR “psychological” OR “psychosocial” OR
“behavioral” OR “behavioral interventions” OR “behavioral therapy” OR
“cognitive” OR “cognitive intervention” OR “mindfulness” OR mindfulness
interventions” AND “bariatric surgery” OR “weight loss surgery” OR “bypass” OR
“gastric sleeve” OR “gastric band”. The literature search was conducted by two
reviewers (PRC and CIFG). The last search was conducted on October 18th,
2019.
Study selection and inclusion criteria
Randomized controlled trials
(RCT) and pretest-posttest studies were included based on the following inclusion
criteria:
1.
Aged
³18
years with a minimum follow-up period equal or greater than four weeks.
2.
Bariatric
surgery patients (patients who underwent bariatric surgery or bariatric surgery
candidates or subjects in a bariatric surgery program).
3.
Studies
that performed pre- or postoperative psychological treatment approaches aimed
to improve MEB.
4.
Studies
that reported pre- and post-intervention outcomes on MEB or problematic eating
patterns, including binge eating, emotional eating, uncontrolled
eating, eating in absence of hunger, night-eating, grazing, snacking, picking
patterns, etc.
Data extraction and quality assessment
All data extraction was
performed by the first author and double-checked by two other authors (CIFG and
MBG). Discrepancies were solved though consultation and consensus. Data was
collected from the full-text articles and was pooled. Data regarding the study
design, sample size, participant’s characteristics (mean age and gender),
follow-up period, retention rate, type of intervention, and outcomes measured
were obtained (Table 1). Data was organized according to the study design (i.e.
RCT and pretest-posttest studies) and by the period of intervention (pre- or
postoperative intervention). Primary outcomes analyzed were MEB and secondary
outcomes were weight loss, anxiety and depression symptoms. When there was more
than one publication of the same study population, the articles where combined
and information was collected from the article that reported the primary
outcomes and that had the longest follow-up. Effect size of the primary
outcomes (MEB) was extracted from the studies when available, when not reported
and data was available, Cohen d effect size was calculated.
Quality of evidence was rated
based on the Grading of Recommendations Assessment, Development and Evaluation
system, that classifies the evidence as high, moderate, low or very low quality(38).
Evidence was divided into primary outcomes (MEB) and secondary outcomes (weight
loss, anxiety and depression symptoms). Quality of the evidence was rated based
on the study design, risk of bias, inconsistency and imprecision of results.
Results
Literature search
The preliminary search
throughout the databases and manual search provided a total of 929 citations.
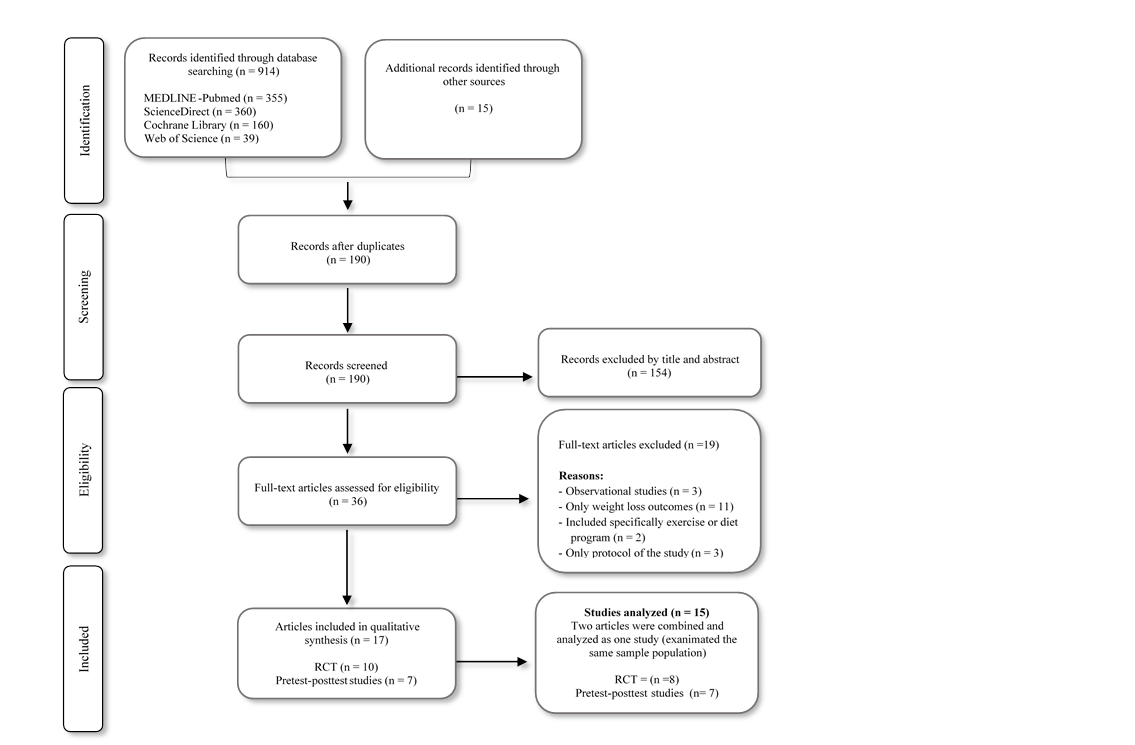
The selection process of the studies is illustrated in a flow diagram (Figure
1).
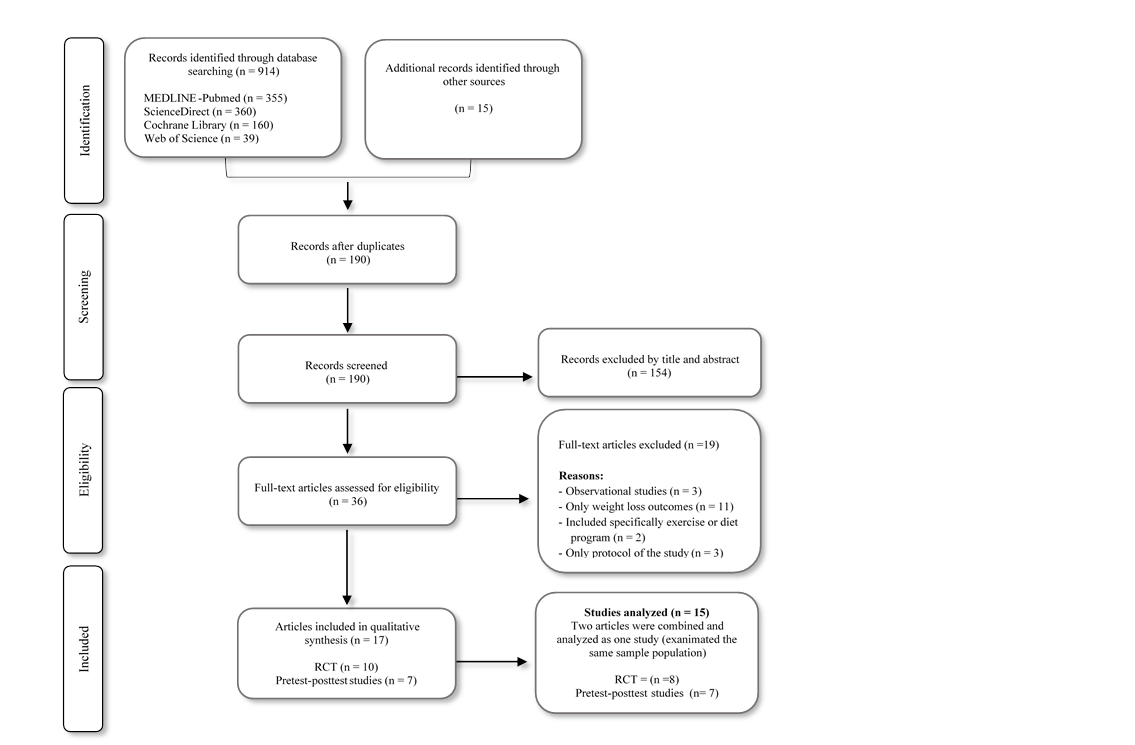
Figure 1. Flow diagram of the study selection process.
Study and participant’s characteristics
A total of 15 studies were
analyzed in this systematic review. Seventeen articles were included, of which
two of these assessed the same sample population in different follow-up
periods. These articles were combined and analyzed as one study. We included
eight randomized controlled trials(39-48) and seven pretest-posttest
studies(31,49-54). Retention rate among the studies ranged from 63%
to 100%. A total of 752 participants were identified from all the studies and sample
size ranged from 7 to 243 participants. Gender distribution was primarily
female (80.3%) and the average participant’s age was 46.1 years (SD ± 6.6).
Follow-up period after intervention ranged from 6 weeks to 48 months. Data
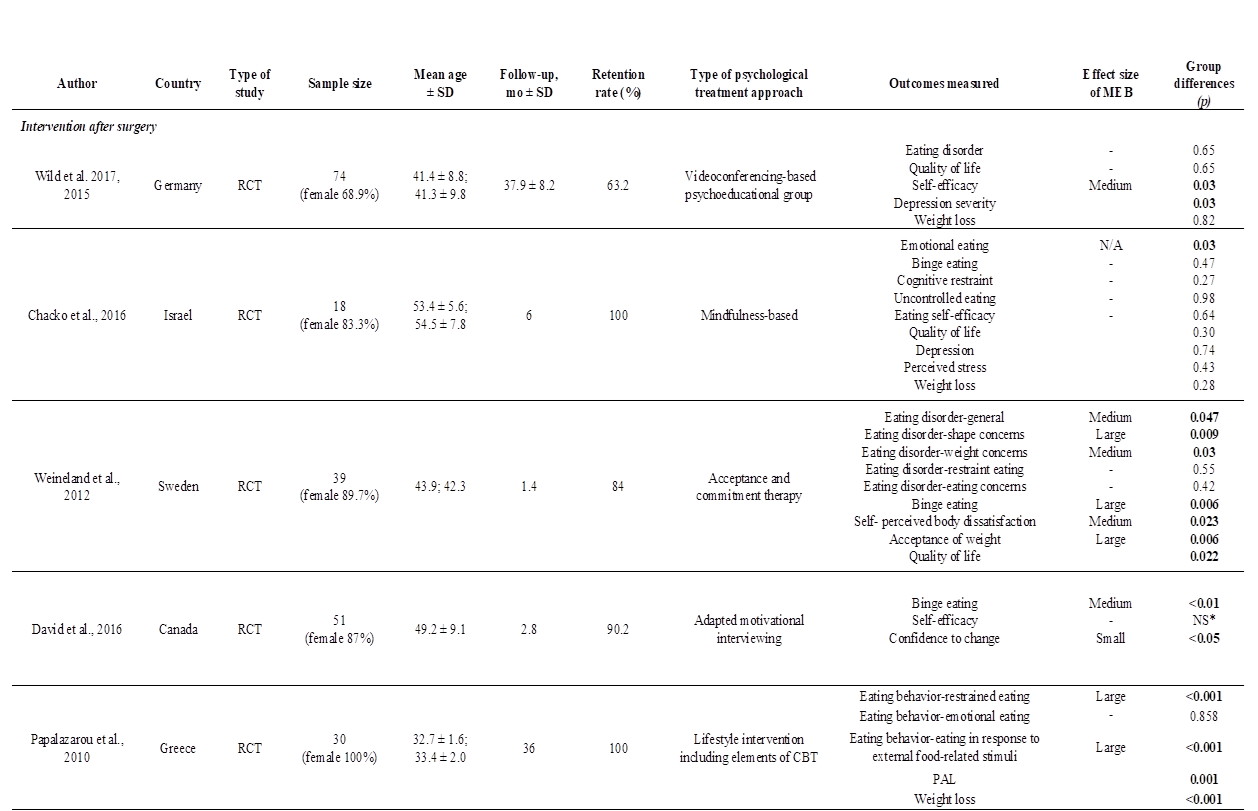
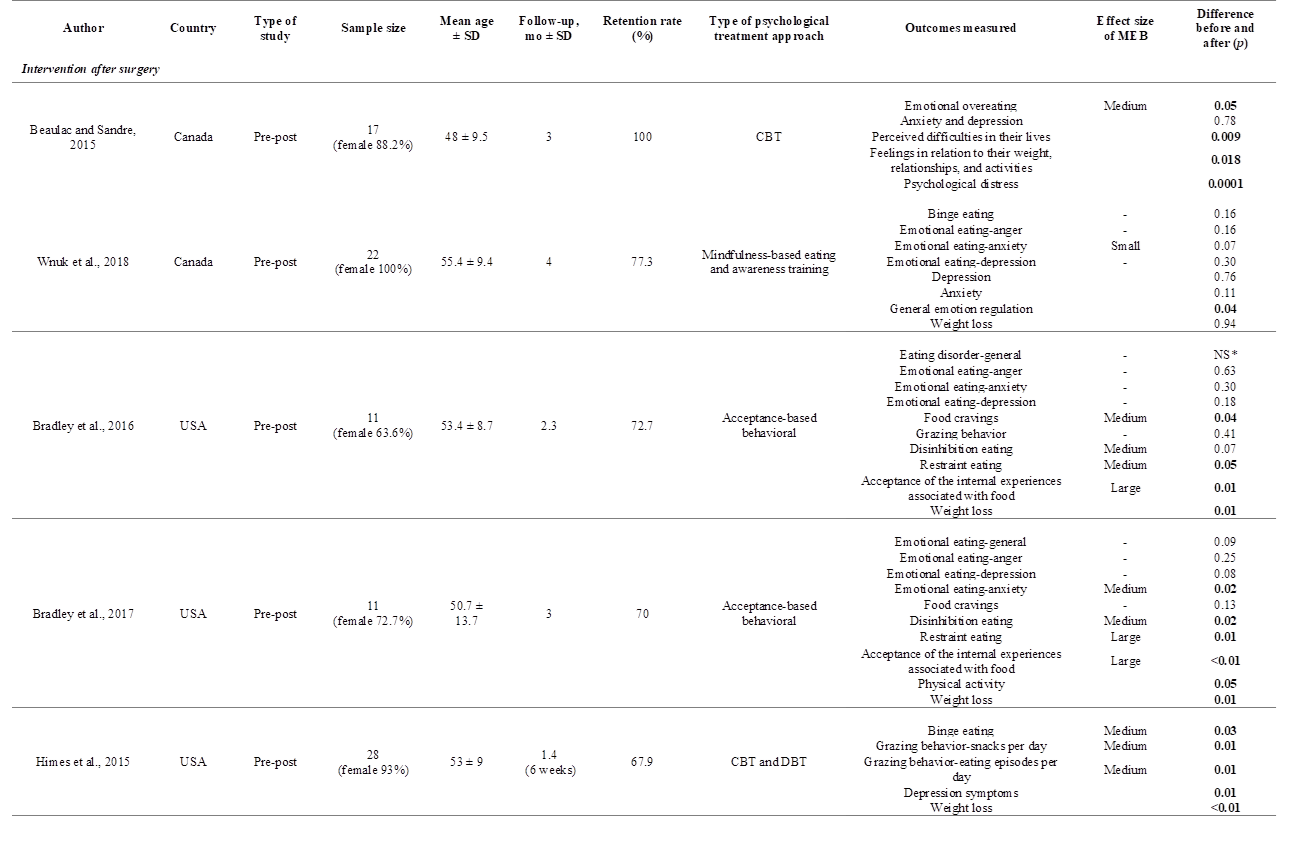
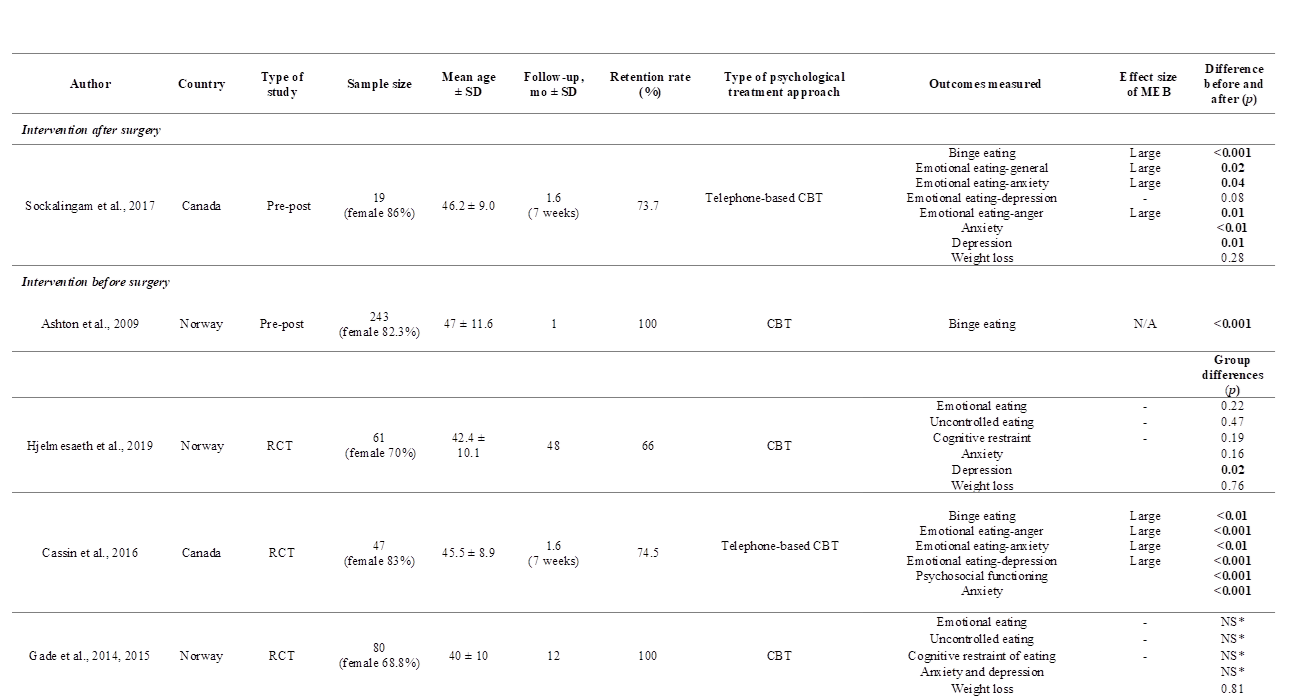
collected from each study is summarized in Table 1.
Table
1. Study characteristics.
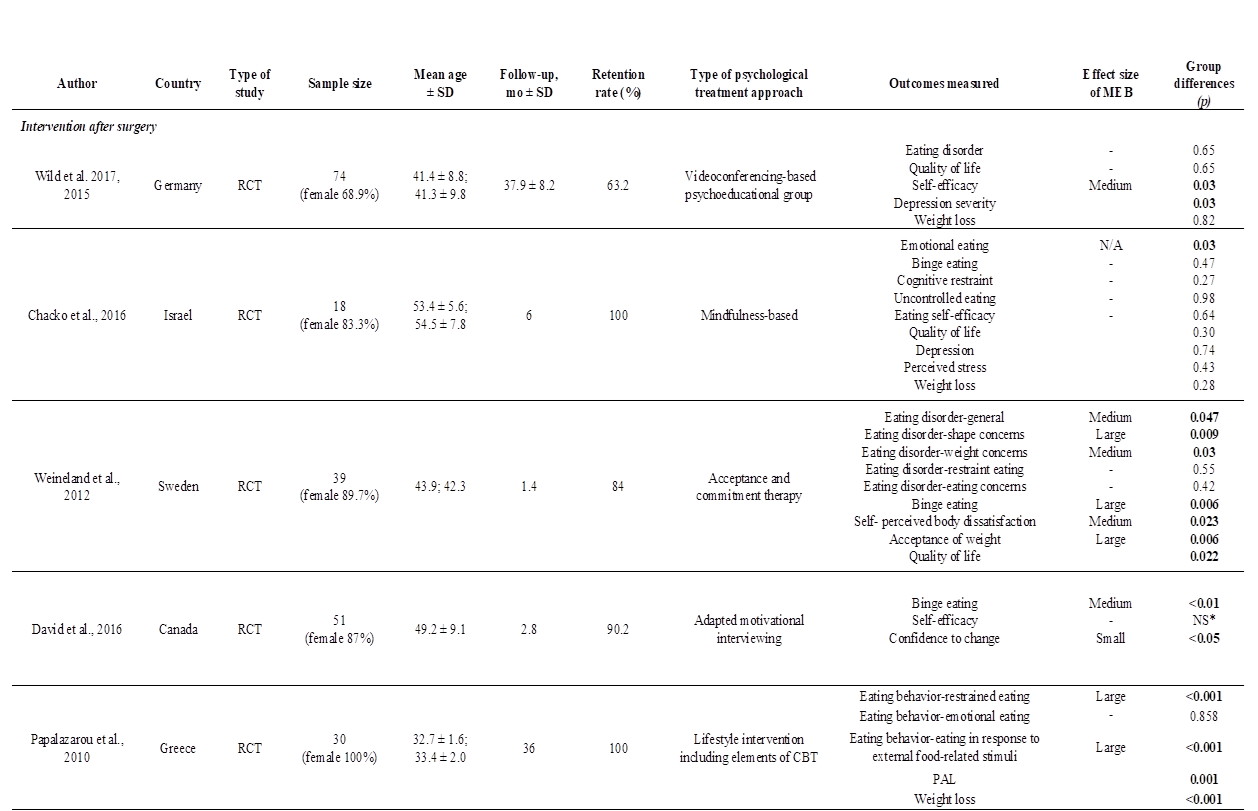
Table
1. (continued)
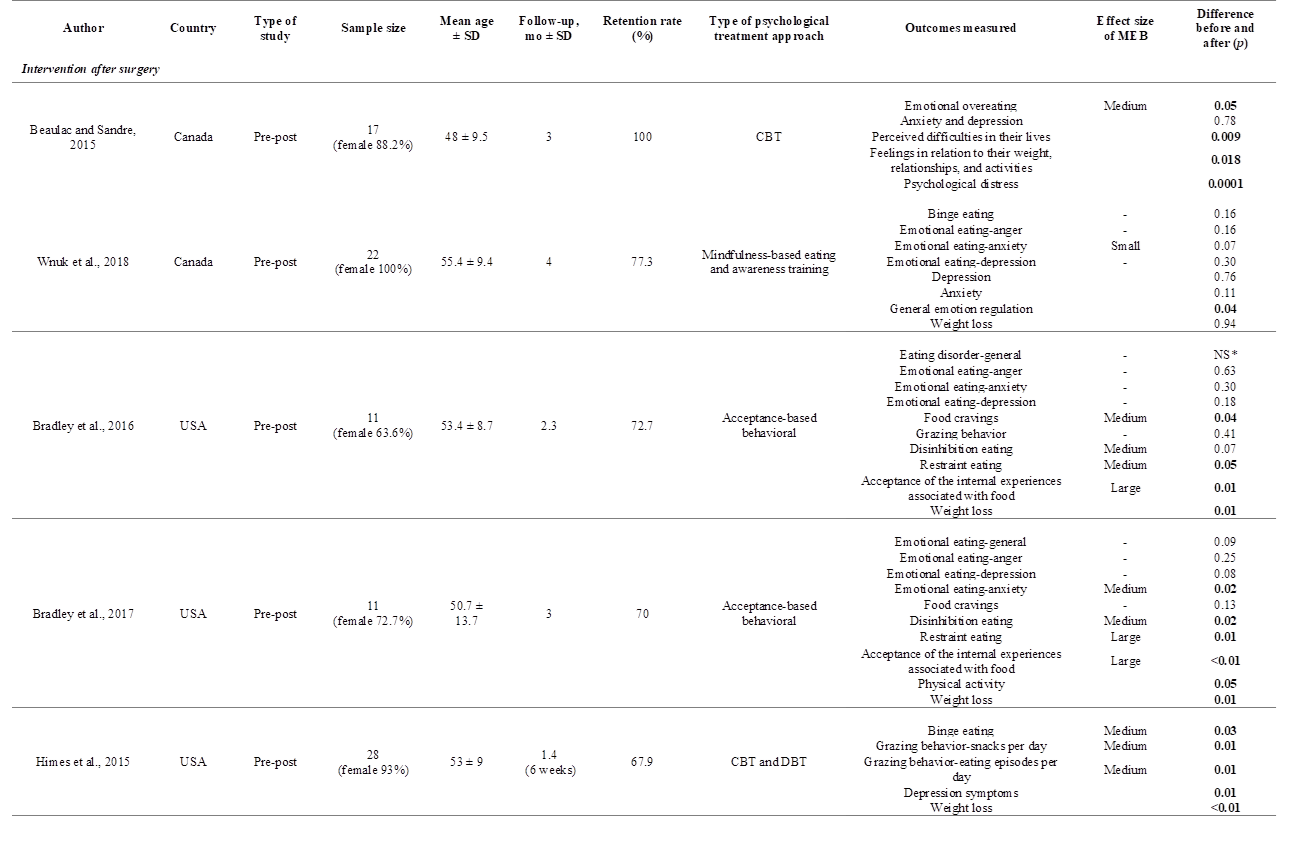
Table
1. (continued)
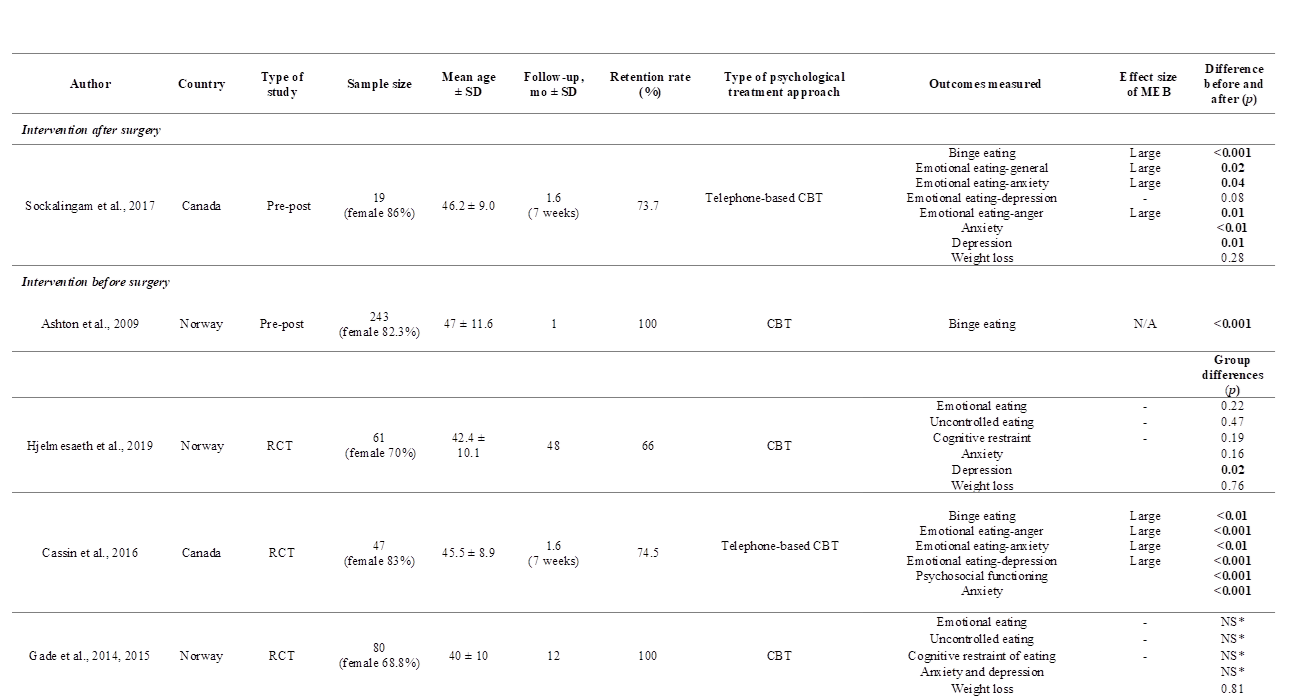
RCT
= randomized control trial; SD = standard deviation; CBT = cognitive-behavioral
therapy; DBT = dialectical behavior therapy; BMI = body mass index; PAL =
physical activity level; NS* = authors did not report p number, but they
reported that p was no significant.; N/A = Not available; - = Not
included since it is not significant.
Psychological treatment approaches
Of the four studies that
assessed the efficacy of preoperative interventions, three were RCT(39,42-44)
and one was pretest-posttest study(49). Of the eleven studies that assessed
postoperative interventions, five were RCT(40,41,45-48) and six were
pretest-posttest studies (31,50-54).
The psychological interventions performed among the studies included were as
follows: cognitive-behavioral therapy (CBT), acceptance-based and acceptance
and commitment therapy, mindfulness-based therapy, psychoeducational group, and
adapted motivational interviewing.
Eight studies included
principles of CBT(31,39,42-45,49,50,53), and two of these were
performed through phone calls(39,53). Two studies included an
acceptance-based behavioral therapy(51,52), and one study an
acceptance and commitment therapy(46). Mindfulness-based therapy was
performed in two studies(40,56). One study performed a
videoconferencing-based psychoeducational group(47,48), and another
study performed adapted motivational interviewing (41).
Primary outcome: Maladaptive eating behaviors
All studies reported the
examination questionnaires used or applied to measure MEB in their
participants. MEB evaluated among the studies included: eating disorders
symptoms (general, restraint, related to shape, weight and eating concerns),
emotional eating (related to anger, anxiety and depression), binge eating,
emotional overeating or uncontrolled eating, disinhibition eating, food
cravings, grazing behaviors, and eating self-efficacy. Other behaviors or
issues related with MEB were evaluated, such as self-perceived body
dissatisfaction, acceptance of weight, confidence of change, and acceptance of
the internal experiences associated with food. The most frequent MEB recorded
among the studies was emotional eating (11 out of 15) followed by binge eating
(8 out of 15).
Overall, all the studies
reported an improvement of MEB. However, some of the studies did not report a
significant effect compared with the control group (RCT) or after the
intervention (pretest-posttest studies). Five out of eight RCT (1 preoperative intervention; 4
postoperative intervention) reported a significant effect (P <0.05)
and four had a medium to large effect size between the groups receiving
psychological intervention and the control group. Six out of seven
pretest-posttest studies (5 postoperative intervention; 1 preoperative intervention)
reported significant difference (P <0.05) and had a small to large
effect size after receiving psychological intervention.
The study conducted by
Hjelmesaeth et al.(44), reported a significant improvement after
psychological intervention compared with the control group of emotional eating
(P= 0.031), uncontrolled eating (P <0.001), and cognitive restraint (P
<0.001). However, these results were reported after a follow-up of 4 months
and after psychological intervention (4 weeks before surgery) and these effects
disappeared after a follow-up of 1 year and 4 years after surgery.
Secondary outcomes: weight loss, anxiety and depression
symptoms
Ten out of 15 studies (four RCT
and five pretest-posttest studies) assessed weight loss. Only one (postoperative intervention)
of the four RCT reported significant (P <0.05) weight loss after
psychological intervention compared with the control group. Three (two
postoperative intervention and one preoperative intervention) out of five
pretest-posttest studies reported significant weight loss difference (P <0.05)
after receiving psychological intervention.
Four pretest-posttest studies (postoperative
intervention), and three RCT (preoperative intervention) assessed anxiety and
depression symptoms. Four studies (three pretest-posttest studies and one RCT)
reported significant improvement in depression symptoms, and two studies (one
pretest-posttest studies and one RCT) reported significant improvement in anxiety
symptoms.
Quality of the evidence
Based on the GRADE system, the
quality of the evidence of the primary outcomes rated from low to moderate.
Seven out of 15 studies included were not randomized controlled trials, and 66%
of the studies presented a follow-up period of less than six months. Four out
of seven RCT had a medium to large effect size. Only four studies assessed MEB
for participant’s recruitment.
Discussion
To our knowledge, this is the
first systematic review aimed to assess psychological intervention approaches
for MEB in bariatric surgery patients. The main finding of this study is that
psychological interventions (regardless of type of therapy performed) have a
positive effect on MEB in bariatric surgery patients at short-term periods.
However, the quality of the evidence rated from low to moderate and the effect
was not sustained after 12 months of follow-up.
Better results were observed
in the studies with a shorter follow-up period. Four studies presented a follow-up
period greater than 12 months and only one showed significant improvement on
MEB. Therefore, the medium and long-term effect of psychological treatment
remain uncertain. The study with the longest follow-up (four years) reported no
clinical effects on MEB at the end of the follow-up period(44). The
immediate effect showed after 10-weeks of psychological treatment disappeared
at the first and fourth year of follow-up. On the other hand, another study
with a follow-up of three years(45), reported significant effects on
MEB after the end of the follow-up. However, this study conducted several
sessions during the three years of follow-up, which suggests that a continuous
intervention might result in a sustained positive effect on MEB.
Two systematic reviews and
meta-analysis have been published, which evaluated the effect of
psychotherapeutic interventions and support groups on weight loss in bariatric
surgery patients(32,33), but they do not include specific assessment
of MEB. These studies showed that those patients attending psychotherapy or
support groups, combined with the surgical treatment, appear to experience
greater weight loss than patients treated with bariatric surgery alone.
The major strengths of this
study are that more than half of the studies were RCTs (eight out of 15), and
almost all of the studies (12 out of 15) presented a relatively high retention
rate (>70 %).
Limitations for this review
are the lack of high-quality studies, the lack of statistical power of the
studies included, the combination of studies with short and medium-term
follow-ups, and the inclusion of a wide variety of psychological treatments.
Additionally, the inconsistency of the results between the studies with similar
follow-up periods might be associated with differences on the assessment of
MEB. Another limitation is that only four studies performed a basal or initial
evaluation of the recruitment of the participants’ sample (31,47,49,50).
The improvement of MEB among
bariatric surgery subjects receiving psychological treatment is small.
Metabolic and bariatric surgery might have a beneficial impact on eating
behaviors; however, this effect does not remain at 12 or more months(42,55).
One study with a follow up of three years shows a positive effect of
psychological treatment when these continue over time, which suggest that long
term interventions are warranted and should be assessed (45).
Conclusion and recommendations
In the present systematic
review positive effects on MEB were shown after psychological treatment at
short-term follow-up. However, the quality of the evidence rated from low to
moderate, and outcomes at ³12 months of follow-up showed no effect on MEB. Continuous
and close monitoring, identification of MEB before and after surgery, and
recurrent supportive pre- and postoperative interventions including
psychotherapy are important to maximize surgical outcomes. Further high-quality
studies are warranted to assess the effect of psychological treatment for MEB
at long-term.
Conflicts of interest
The authors
declare that there is no conflict of interest regarding the publication of this
paper.
Referencias
1.
M. Ng, T. Fleming, M. Robinson, et al.,
"Global, regional, and national prevalence of overweight and obesity in
children and adults during 1980–2013: a systematic analysis for the Global
Burden of Disease Study 2013," The Lancet, vol. 384, no. 9945,
pp.766-81, 2014.
2.
World Health Organization, "Obesity and
overweight 2018," (Available from: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight).
3.
C.M. Hales, M. D. Carroll, C. D. Fryar, C. L.
Ogden, "Prevalence of Obesity Among Adults and Youth: United States,
2015–2016," NCHS Data Brief, vol. 288, pp. 1-8, 2017.
4.
E. P. Williams, M. Mesidor, K. Winters, P. M.
Dubbert, S. B. Wyatt, "Overweight and Obesity: Prevalence, Consequences,
and Causes of a Growing Public Health Problem," Current obesity reports,
vol. 14, no. 3, pp. 363-70, 2015.
5.
M. Fried, V. Yumuk, J. M. Oppert, et al.,
"Interdisciplinary European Guidelines on Metabolic and Bariatric Surgery,"
Obes Surg, vol. 24, no. 1, pp. 42-55, 2014.
6.
National Heart, Lung, and Blood Institute -
NIH, "Clinical guidelines on the identification, evaluation, and treatment
of overweight and obesity in adults: the evidence report Rockville, Md:
National Heart, Lung, and Blood Institute," 1998.
7.
I. Rasera Jr, A. Luque, S.M. Junqueira Jr, N.
C. Brasil, P. C. Andrade, "Effectiveness and Safety of Bariatric Surgery
in the Public Healthcare System in Brazil: Real-World Evidence from a
High-Volume Obesity Surgery Center," Obes Surg, vol. 27, no. 2, pp.
536-40, 2017.
8.
N. Puzziferri, T. B. Roshek 3rd, H. G. Mayo,
R. Gallagher, S. H. Belle, E. H. Livingston, "Long-term follow-up after
bariatric surgery: a systematic review," JAMA, vol. 312, no. 9, pp.
934-42, 2014.
9.
S. H. Chang, C. R. Stoll, J. Song, J.E Varela,
C. J. Eagon, G. A, Colditz, "The effectiveness and risks of bariatric
surgery: an updated systematic review and meta-analysis, 2003-2012," JAMA
surgery, vol. 149, no. 3, pp. 275-87, 2014.
10.
M. Khosravi-Largani, M. Nojomi, R. Aghili, et
al., "Evaluation of all Types of Metabolic Bariatric Surgery and its
Consequences: a Systematic Review and Meta-Analysis," Obes Surg,
vol. 29, no. 2, pp. 651-690, 2019.
11.
P. Ruiz-Cota, M. Bacardi-Gascon, A.
Jimenez-Cruz A, "Long-term outcomes of metabolic and bariatric surgery in
adolescents with severe obesity with a follow-up of at least 5 years: A
systematic review," Surg Obes Relat Dis, vol. 15, no. 1, pp.
133-144, 2019.
12.
P.E. O'Brien, A. Hindle, L. Brennan, et al.,
"Long-Term Outcomes After Bariatric Surgery: a Systematic Review and
Meta-analysis of Weight Loss at 10 or More Years for All Bariatric Procedures
and a Single-Centre Review of 20-Year Outcomes After Adjustable Gastric
Banding," Obes Surg, vol. 29, no. 1, pp. 3-14, 2019.
13.
Z. Khorgami, S. Shoar , A. A. Saber, C. A.
Howard, G. Danaei, G. M. Sclabas, "Outcomes of Bariatric Surgery Versus
Medical Management for Type 2 Diabetes Mellitus: a Meta-Analysis of Randomized
Controlled Trials," Obes Surg, vol. 29, no. 3, pp. 964-974, 2019.
14.
J. P. Mann, A. D. Jakes, J. D. Hayden, J. H.
Barth, "Systematic review of definitions of failure in revisional
bariatric surgery," Obes Surg, vol. 25, no. 3, pp. 571-4,
2015.
15.
American Society for Metabolic and Bariatric
Surgery, "Bariatric Surgery Misconceptions," (Available from:
https://asmbs.org/patients/bariatric-surgery-misconceptions).
16.
M. Livhits, C. Mercado, I. Yermilov, et al.,
"Behavioral factors associated with successful weight loss after gastric
bypass," Am Surg, vol. 76, no. 10, pp. 1139-42, 2010.
17.
L. Salem, C. C. Jensen, D. R. Flum, "Are
bariatric surgical outcomes worth their cost? A systematic review," J
Am Coll Surg, vol. 200, no. 2, pp. 270-8, 2005.
18.
N. J. Switzer, S. Karmali, R. S. Gill, V.
Sherman, "Revisional Bariatric Surgery," Surg Clin North Am,
vol. 96, no. 4, pp. 827-42, 2016.
19.
G. M. Campos, C. Rabl, K. Mulligan, et al.,
"Factors associated with weight loss after gastric bypass," Arch Surg,
vol. 143, no. 9, pp. 877-83, 2008.
20.
D. B. Sarwer, T. A. Wadden, A. N. Fabricatore,
"Psychosocial and behavioral aspects of bariatric surgery," Obes
Res, vol. 13, no. 4, pp. 639-48, 2005.
21.
A. Maleckas, R. Gudaitytė, R. Petereit, L.
Venclauskas, D. Veličkienė, "Weight regain after gastric bypass: etiology
and treatment options," Gland surgery, vol. 5, no. 6, pp. 617-24,
2016.
22.
J. Odom, K. C. Zalesin, T. L. Washington, et
al., "Behavioral Predictors of Weight Regain after Bariatric
Surgery," Obes Surg, vol. 20, no. 3, pp. 349-56, 2010.
23.
J. E. Mitchell, W. C. King, A. Courcoulas, et
al., "Eating behavior and eating disorders in adults before bariatric
surgery," Int J Eat Disord, vol. 48, no. 2, pp. 215-22, 2015.
24.
E. Conceição, J. E. Mitchell, A. R. Vaz, et
al., "The presence of maladaptive eating behaviors after bariatric surgery
in a cross sectional study: Importance of picking or nibbling on weight
regain," Eating Behaviors, vol. 15, no. 4, pp. 558-62, 2014.
25.
A. Pinto-Bastos, M. de Lourdes, I. Brandão, P.
P. P Machado, E .M Conceição, "Weight loss trajectories and
psychobehavioral predictors of outcome of primary and reoperative bariatric
surgery: a 2-year longitudinal study," Surg Obes Relat Dis, vol.
15, no. 7, pp. 1104-112, 2019.
26.
M. A. Kalarchian, W. C. King, M. J. Devlin, et
al., "Psychiatric Disorders and Weight Change in a Prospective Study of
Bariatric Surgery Patients: A 3-Year Follow-Up," Psychosom Med, vol.
78, no. 3, pp. 373-81, 2016.
27.
C. S. Brode, J.E. Mitchell, "Problematic
Eating Behaviors and Eating Disorders Associated with Bariatric Surgery," Psychiatr
Clin North Am, vol. 42, no. 2, pp. 287-97, 2019.
28.
M. A. Kalarchian, M. D. Marcus, M.D. Levine,
et al., "Psychiatric disorders among bariatric surgery candidates:
relationship to obesity and functional health status," Am J Psychiatry,
vol. 164, no. 2, pp. 328-34, 2007.
29.
G. A. Williams-Kerver, K. J. Steffen, J. E.
Mitchell, "Eating Pathology After Bariatric Surgery: an Updated Review of
the Recent Literature," Current psychiatry reports, vol. 21, no. 9,
pp. 86, 2019.
30.
L. R. Miller-Matero, K. Bryce, C. K. Saulino,
K. E. Dykhuis, J. Genaw, A. M. Carlin, "Problematic Eating Behaviors
Predict Outcomes After Bariatric Surgery," Obes Surg, vol. 28, no.
7, pp. 1910-5, 2018.
31.
S. M. Himes, K. B. Grothe, M. M. Clark, J. M.
Swain, M. L. Collazo-Clavell, M. G. Sarr, "Stop regain: a pilot
psychological intervention for bariatric patients experiencing weight
regain," Obes Surg, vol. 25, no. 5, pp. 922-7, 2015.
32.
N. N. Beck, M. Johannsen, R. K. Stoving, M.
Mehlsen, R. Zachariae, "Do postoperative psychotherapeutic interventions
and support groups influence weight loss following bariatric surgery? A
systematic review and meta-analysis of randomized and nonrandomized
trials," Obes Surg, vol. 22, no. 11, pp. 1790-7, 2012.
33.
A. Rudolph, A. Hilbert, "Post-operative
behavioural management in bariatric surgery: a systematic review and
meta-analysis of randomized controlled trials," Obes Rev, vol. 14,
no. 4, pp. 292-302, 2013.
34.
F. Stewart, A. Avenell, "Behavioural
Interventions for Severe Obesity Before and/or After Bariatric Surgery: a
Systematic Review and Meta-analysis," Obes Surg, vol. 26, no. 6,
pp. 1203-14, 2016.
35.
J. A. Brewer, A. Ruf, A. L. Beccia, et al.,
"Can Mindfulness Address Maladaptive Eating Behaviors? Why Traditional
Diet Plans Fail and How New Mechanistic Insights May Lead to Novel
Interventions," Front Psychol, vol. 9, pp. 1418, 2018.
36.
A. Wenzel, "Basic Strategies of Cognitive
Behavioral Therapy2," Psychiatr Clin North Am, vol. 40, no. 4, pp.
597-609, 2017.
37.
D. Moher, L. Shamseer, M. Clarke, et al.,
"Preferred reporting items for systematic review and meta-analysis
protocols (PRISMA-P) 2015 statement," Syst Rev, vol. 4, no. 1,
2015.
38.
GRADE Work Group, "Grading quality of
evidence and strength of recommendations," BMJ, vol. 328, no. 7454,
pp. 490, 2004.
39.
S. E. Cassin, S. Sockalingam, C. Du, S. Wnuk,
R. Hawa, S. V. Parikh, "A pilot randomized controlled trial of
telephone-based cognitive behavioural therapy for preoperative bariatric
surgery patients," Behav Res Ther, vol. 80, pp. 17-22, 2016.
40.
A. S. Chacko, G. Y. Yeh GY, R. B. Davis, C. C.
Wee, "A mindfulness-based intervention to control weight after bariatric
surgery: Preliminary results from a randomized controlled pilot trial," Complement
Ther Med, vol. 28, pp. 13-21, 2016.
41.
L. A. David, S. Sockalingam, S. Wnuk, S. E.
Cassin, "A pilot randomized controlled trial examining the feasibility,
acceptability, and efficacy of Adapted Motivational Interviewing for post-operative
bariatric surgery patients," Eat Behav, vol. 22, pp. 87-92, 2016.
42.
H. Gade, O. Friborg, J. H. Rosenvinge, M. C
Smastuen, J. Hjelmesaeth J, "The Impact of a Preoperative Cognitive
Behavioural Therapy (CBT) on Dysfunctional Eating Behaviours, Affective
Symptoms and Body Weight 1 Year after Bariatric Surgery: A Randomised
Controlled Trial," Obes Surg, vol. 25, no. 11, pp. 2112-9, 2015.
43.
H. Gade, J. Hjelmesæth, J. H. Rosenvinge, O.
Friborg, "Effectiveness of a Cognitive Behavioral Therapy for Dysfunctional
Eating among Patients Admitted for Bariatric Surgery: A Randomized Controlled
Trial," J Obes, 2014.
44.
J. Hjelmesaeth, J. H. Rosenvinge, H. Gade, O.
Friborg, "Effects of Cognitive Behavioral Therapy on Eating Behaviors,
Affective Symptoms, and Weight Loss After Bariatric Surgery: a Randomized
Clinical Trial," Obes Surg, vol. 29, no. 1, pp. 61-9, 2019.
45.
A. Papalazarou, M. Yannakoulia, S. A.
Kavouras, et al., "Lifestyle intervention favorably affects weight loss
and maintenance following obesity surgery," Obesity (Silver Spring, Md),
vol. 18, no, 7, pp. 1348-53, 2010.
46.
S. Weineland, D. Arvidsson, T. P Kakoulidis,
J. Dahl, "Acceptance and commitment therapy for bariatric surgery
patients, a pilot RCT," Obes Res Clin Pract, vol. 6, no. 1, pp.
e1-e90, 2012.
47.
B. Wild, K. Hunnemeyer, H. Sauer H, et al.,
"A 1-year videoconferencing-based psychoeducational group intervention
following bariatric surgery: results of a randomized controlled study," Surg
Obes Relat Dis, vol. 11, no. 6, pp. 1349-60, 2015.
48.
B. Wild, K. Hunnemeyer, H. Sauer, et al.,
"Sustained effects of a psychoeducational group intervention following
bariatric surgery: follow-up of the randomized controlled BaSE study," Surg
Obes Relat Dis, vol. 13, no. 9, pp. 1612-8, 2017.
49.
K. Ashton, M. Drerup, A. Windover, L. Heinberg,
"Brief, four-session group CBT reduces binge eating behaviors among
bariatric surgery candidates," Surg Obes Relat Dis, vol. 5, no. 2,
pp. 257-62, 2009.
50.
J. Beaulac, D. Sandre, "Impact of a CBT
psychotherapy group on post-operative bariatric patients," SpringerPlus,
vol. 4, pp. 764, 2015.
51.
L. E. Bradley, E. M Forman, S. D. Kerrigan, M.
L. Butryn, J. D. Herbert, D. B. Sarwer, "A Pilot Study of an
Acceptance-Based Behavioral Intervention for Weight Regain After Bariatric
Surgery," Obes Surg, vol. 26, no. 10, pp. 2433-41, 2016.
52.
L. E. Bradley, E. M. Forman, S. G. Kerrigan,
et al., "Project HELP: a Remotely Delivered Behavioral Intervention for
Weight Regain after Bariatric Surgery," Obes Surg, vol. 27, no. 3,
pp. 586-98, 2017.
53.
S. Sockalingam, S. E. Cassin, S Wnuk, et al,
"A Pilot Study on Telephone Cognitive Behavioral Therapy for Patients
Six-Months Post-Bariatric Surgery," Obes Surg, vol. 27, no.
3, pp. 670-5, 2017.
54.
S. M. Wnuk, C. M. Du, J. Van Exan, et al.,
"Mindfulness-Based Eating and Awareness Training for Post-Bariatric
Surgery Patients: a Feasibility Pilot Study," Mindfulness, vol. 9,
no. 3, pp. 949-60, 2018.
55.
C. L. Wimmelmann, F. Dela, E. L. Mortensen,
"Psychological predictors of weight loss after
bariatric surgery: A review of the recent research," Obes Res Clin
Pract, vol. 8, no. 4, pp. e299-e313, 2014.