ORIGINAL (English version)
A switch to the Duodenal Switch
Cambiar al Cruce bariátrico. A switch to the switch
Aniceto Baltasar, Nieves Pérez, Rafael Bou, Marcelo Bengochea, Carlos Serra
Alcoy County Hospital and San Jorge Clinic. Alcoy, Alicante, Spain
* Autor para correspondencia.
![]()
This work is licensed
under a Creative
Commons
Attribution-NonCommercial-ShareAlike 4.0 International License
La revista no cobra tasas por el envío de trabajos,
Abstract
Background. Duodenal Switch (DS) is a procedure that combines a Sleeve-Forming Gastrectomy (SFG) plus a biliopancreatic diversion (BPD) for the treatment of morbid obesity (MO) with a higher weight loss and resolution of comorbidities
Objectives. Report our experience with 950 consecutive DS operations performed from 1994 to 2016.
Setting. Mix of teaching and private institution in a county hospital of Spain.
Methods. We report an observational, retrospective and longitudinal study of 950 consecutive morbidly obese patients treated by DS surgery.
Results. We performed 518 open and 432 laparoscopic DS. Operative mortality was 0.84% (1.38% in DS and 0.38% in LDS), 4.84% had leaks, two had hepatic failures (0.2%) and malnutrition was present in 3.1%. At 5 years, the percentage of BMI lost was 80%, and percentage of expected BMI loss was more than 100%.
Conclusions. DS is the most aggressive bariatric surgery (BS) technique, but with the best long-term weight loss. We describe operative complications and long-term follow-up guidelines.
Keywords
Morbid obesity; Duodenal Switch; Bariatric surgery; Sleeve-Forming Gastrectomy; Biliary pancreatic diversion; Weight loss
Resumen
Introducción. El Cruce duodenal (CD) es un procedimiento bariátrico que combina una gastrectomía vertical (GV) y una derivación bilio-pancreática (DBP) y consigue la mayor pérdida de sobreso perdido (PSP) a largo plazo y resolución de comorbilidades.
Objetivos. Presentamos nuestra experiencia sobre 950 pacientes CD tratados desde 1994 a 2011 de obesidad mórbida (OM) desde 1994 a 2011 y 27 años de seguimiento en Hospital Comarcal de enseñanza e Institución Privada de España.
Métodos. Estudio observacional, retrospectivo y longitudinal de 950 pacientes consecutivos tratados con cirugía de CD.
Resultados. Hubo 518 CD abiertos (CDA) y 432 CD laparoscópicos (CDL). Mortalidad operatoria del 0,84% (1,38% en CDA y 0,38% en CDL), 4,84% incidencia de fugas, dos insuficiencia hepática (0,2%) y desnutrición calórico proteica (DCP) en el 3,1%. A los 5 años, pérdida de del 80% de IMC y PSP de 90% y % perdido del IMC esperado del 100%.
Conclusiones. El CD es la técnica bariátrica más agresiva, y con la mejor pérdida de peso a largo plazo. Se describen las complicaciones operatorias y las pautas de seguimiento a largo plazo. Y se propone un cambio para aceptar esta terapia.
Palabras clave
Obesidad mórbida; Cruce duodenal; Cirugía bariátrica; Gastrectomía Vertical; Derivación bilio-pancreática; Pérdida de peso
Introduction
Duodenal
Switch (DS) surgery consists of two operations, Sleeve-forming
Gastrectomy (SFG) plus a Biliopancreatic diversion (BPD). It is the most
complex technique in bariatric surgery (BS). DS combines restriction
of food-intake and malabsorption in the small bowel.
Doug Hess (1) initiated the DS in 1988 and described the three main components: 1) SFG to remove most of the stomach at the greater curvature, which reduces gastric volume but allows normal emptying; 2) Post pyloric division of the duodenum [D1] to allow emptying into the small bowel thru a Duodenal ileal anastomosis (DIA). 3) Diversion of 50% of proximal small bowel to cause malabsorption.
Hess (2) measures the entire small intestine, at low bowel tension, from ligament of Treitz to the ileocecal valve and uses 50% of its length as Biliopancreatic Loop (BPL), 40% as Alimentary Loop (AL) and 10% as Common Loop (CL).
Marceau (3) used the standard BPD until 1991 and one year later he changed to DS and he was the first to publish it the DS (4) as parietal gastrectomy plus BPD and compared 252 DBP with distal gastrectomy and 465 CD with a 1.7% operative mortality. Lagacé (5) reported in 1995 the first good CD results in 61 patients with a new type of gastrectomy. Hess (6) uses a suture to invert the gastric serosa and cover the SFG staples and avoid leakage in the line of staples. Baltasar (7,8) describes the gastric part of the operation as SFG (7,8).
The CD (9-18) was considered a standard technique in the 90´s (Figure 1). Ren (19) made the first CDL in October 1999 and Baltasar (20-24) describes the first CDL in Europe in 2000 (25). Paiva (26) in Brazil and Scopinaro (27) in Italy initiate in 2000 the standard laparoscopic DBP.
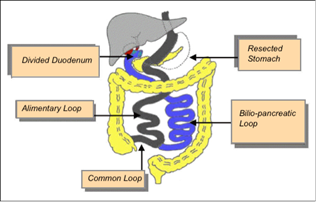
Figure 1. Duodenal Switch = SFG plus BPD
To measure weight loss results the Quetelet Body Mass Index (BMI) is used. BMI = kg/m2, but… after reviewing 7,410 patients our mathematician developed the concept of predictive or expected BMI (28) to calculate BMI as Initial BMI (IBMI) any BMI superior to 25 and make the calculation not from IBMI but of IBMI in excess of 25. The % of excess weight lost (%EWL) are not equal in a MO patient grade 2 compared with the ones with triple obesity. Molina has reported that the expected BMI is useful (29)
Operative techniques
DS by Open Laparotomy (ODS)
The patient is in Trendelenburg position. A supraumbilical transverse incision Is made between the two coastal margins (Figures 2 a-b). The round and triangular ligaments are sectioned. The gallbladder and appendix are removed. The open transverse approach gives better exposure and fewer hernias than the average laparotomy, but since laparoscopy its use today is restricted to re-operations.

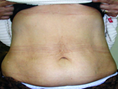

Figure 2. a) incision; b) Invisible Scar; c) Supra pubic dermo lipectomy
The abdomen is closed in two layers of continuous Maxon. After weight loss, the scar shortens by one third in length (Figure 2b) and allows the superior wound to reach the pubic area in the abdominoplasty at the body contour surgery (Figure 2c). We started the ODS on 17.03.1994 with surgical times of 91 minutes.
Laparoscopic CD (LDS)
It's done by three surgeons. Six ports are used (Figure3). The Optical Trocar or "main port" is Ethicon # 12, enters. It enters the abdomen under vision at the lateral edge of the right rectus, three fingers below the costal margin. A 10 mm central supraumbilical port is used for the mid-line camera.

Figure 3. Position of ports
There are four 5 mm ports, two sub-costal located on the right and left, one in the left hypochondrium and the other in the epigastrium used to retract the liver (Figure 3). To avoid slippage, we use Termanian trocars.
The entire small intestine is measured from the ileocecal valve to Treitz. The CL is marked with a clip. The AL is divided with linear stapler. The BPL starts at the first part of the duodenum (D1) joins at the union of AL-CL as end-lateral Roux-Y (RY) jejunal-ileal anastomosis (JIA) with a continuous monoplane resorbable suture. The mesenteric defect is closed with a non-absorbable suture.
The greater gastric curvature vascular supply is divided starting 3 cm distal to the pylorus and up to the angle of His. A 12 mm nasogastric probe is passed along the inner curvature of the stomach and used as a guide to divide the stomach sequentially with linear staplers starting at the pylorus. Then both gastric walls, posterior and anterior to the line of staples joins with the omentum with a continuous inverting suture to avoid torsion and leakage of the gastric tube.
A retro-duodenal tunnel is created in D1, distal to the right gastric artery, which allows the duodenal division with a linear stapler before the Oddi sphincter. The distal duodenal stump is also reinforced with continuous inverting suture.
The proximal AL passes retro-colic, on the right, and a Duodenum-Ileal Anastomosis (DIA) is performed. The operation has four sutures-lines (gastric reinforcement, DIA, jejunum-ileal RY anastomosis and the distal duodenal stump) and drainages are placed, one next to the gastric tube and the other in DIA.
All anastomoses are hand-sutured with a monolayer continuous suture. All sutures start with the sliding and self-blocking knot of Serra-Baltasar (30-31) and end with Cuschieri one (32). The intestine is measured with forceps at 5 cm steps to avoid lesions of the intestinal serosa.
The stomach is removed without a protective bag. A Maxon suture closes the 12 mm port fascia to prevent hernias. We started the LDS on 10.5.2000 (20). The average operative time was 155 ' after the first 50 cases.
At discharge, patients received prescriptions with vitamin A complex 20.000 UI, vitamin D 50.000 IU, calcium carbonate 1000 mg and ferrous sulfate 300, vitamins B1 and B2
Material and Methods
950 consecutive MO patients (518 open and 432 laparoscopic) have been operated from 1994 to 2011, after a complete multidisciplinary preoperative evaluation and legal informed consent. 782 were women (82.3%) and 168 men (17.7%). The average age was 35 years (24-63). 474 were foreigners (361 US citizens, 17 from Canada, 73 from Norway and 25 from England) were intervened by the same team at the private center.
The average Initial BMI (IBMI) (Kg/m2) was 49.23 (Women-49.26 and Men-49.07). Obesity Range: a) Obesity, Grade 2 with comorbidities (IMCI < 40), 110 patients (mean 37.66); b) Morbidly Obese (MO) (IMCI 40-50), 464 patients (mean 45.11); c) Super-Obese (SO) (BMI 50-60), 272 patients (mean 54.32) and D) Super/Super Obesity (SSO) IBMI > 60, 104 patients (mean > 66.50) and a patient had IBMI-100.
Comorbidities: 115 patients suffered diabetes mellitus Type 2 (DM2), 103 hypertension, 5 heart disease, 62 dyslipidemia, 19 Obstructive pulmonary disease, 16 osteoarthritis, 1 pseudo brain tumor.
Results
Main intraoperative complications
Three patients needed tracheostomy due to a failure of oral intubation and severe desaturation, without incidents.
In three patients, the 12 mm gastric tube did not pass past the esophageal-gastric junction and stapling of the stomach was done under visual control.
Surgical mortality at 30 days occurred in six ODS patients (1.38%). The causes were: a) Leak in ADI - 1; b) Leak in RY, rhabdomyolysis and multiorgan failure - 1; c) Pulmonary embolism - 2; d) Leak in duodenal stump - 1; e) Leak in His angle - 1. Two LDS patients died (0.38%) by pulmonary emboli. The average mortality of both groups was 0.84%.
Postoperative Morbidity
1.Leaks. There were 46 Leaks for a total leak rate of 4.84%.
a) Leakage in his angle of His: 21 cases (2.3% incidence). 10 were treated with endoprosthesis, drainage or laparotomy and 3 with RY shunt. One of them died.
b) Leakage of the duodenal stump. One patient suffered a leak in the duodenal stump, it was repaired but died of sepsis. Since then, we have protected all staple-lines with an inverting suture and there were no more leaks.
c) DIA Leakage: 24 cases (2.5% incidence). This the most difficult anastomosis. 19 of them suffered early leaks, were successfully treated with drainage or re-do anastomosis, five cases had late leaks (up to 2-14 years later) and at re-operation the anastomosis was redone. In one case, the leak occurred 3 years after the intervention, as a gastro-pleural fistula and was treated with total gastrectomy.
d) RY leak. A patient had a small intestine diverticulum 110 cm from the ileocecal valve, and it was removed, and an open RY performed at the site without incident. There was a leakage and the diagnostic radiological tests did not clarify the cause, and with late diagnosis, he was re-operated and suffered rhabdomyolysis and multiple organ failure and died.
2. Pulmonary embolism. Two patients with IBMI-70 and IBMI-65 had embolism despite prophylactic therapy and died. Deep vein thrombosis in another case was successfully treated.
