REVIEW (English version)
Effectiveness of diagnostic testing for Cervical Cancer and Human Papilloma Virus
Eficacia de las pruebas diagnósticas del Cáncer Cervicouterino y Virus del Papiloma Humano
José Eduardo Samperio Calderón1, Arturo Salazar Campos2
1 Maestro en Salud Publica, Universidad Autonoma del Estado de Hidalgo, Pachuca, Hidalgo. México
2 Maestro en Salud Publica, Universidad Autonoma del Estado de Hidalgo, Pachuca, Hidalgo. México
* Autor para correspondencia.
![]()
This work is licensed under
a Creative
Commons
Attribution-NonCommercial-ShareAlike 4.0 International License
La revista no cobra tasas por el envío de trabajos,
Abstract
Cervical cancer is one of the first 5 most common neoplasms in women in the world, derived from this over time that screening tests have emerged for its timely diagnosis (conventional cytology, liquid based cytology, visual inspection with acid acetic or Lugol, colposcopy ...); These tests have been perfected and even created. The detection reactions of causative agents (human papilloma virus) such as hybridization and PCR (polymerase chain reaction). As a result of this review, the use of screening tests such as conventional cytology, inspection with acetic acid or Lugol derived from its sensitivity and specificity that can lead to false positives in the diagnoses is negative or erroneous; This is true in cervical lesions or cervical cancer.
Keywords
Cervical cáncer; human papilloma virus; screening; efficacy
Resumen
El cáncer de cuello uterino es una de las primeras 5 neoplasias más comunes en mujeres en el mundo, derivado de esto a través del tiempo han surgido pruebas de tamizaje para su diagnóstico oportuno (citología convencional, citología a base liquida, inspección visual con ácido acético o Lugol, colposcopia…); dichas pruebas se han perfeccionado e incluso se han creado nuevas que permiten la detección del agente causal (virus del papiloma humano) como la hibridación y PCR (reacción de cadena de polimerasa), cada herramienta de detección tiene diferente sensibilidad y especificidad; como resultado de este revisión, es negativo o erróneo el uso de pruebas de tamizaje como citología convencional, inspección con ácido acético o Lugol derivado de su sensibilidad y especificidad que pueden originar falsos positivos en los diagnósticos; esto en cuanto a lesiones cervicales o cáncer cervicouterino.
Palabras clave
Cáncer Cervicouterino; virus del papiloma humano; tamizaje; eficacia
Abbreviations
ASCUS Atypical cells of undetermined significance
CCU Cervical cancer
DNA Deoxyribonucleic acid
HPV Human papilloma virus
IVL Visual inspection after applying the yodoyodurada of Lugol's solution
LIEA High-grade intraepithelial lesions
LIEB Intraepitelilaes of low-grade lesions
NIC Cervical intraepithelial neoplasia
NOM Mexican Official Standard
PCR Polymerase chain reaction
RNA Ribonucleic acid
RPM Revolutions per minute
SSA Secretariat of Health
VAT Visual inspection after application of acetic acid
Introduction
Cervical cancer is the seventh most frequent neoplasm in the world population and the fourth most frequent among women with an estimated 528 thousand new cases diagnosed annually, 85% of which are recorded in developing countries. The incidence is higher in developing countries; varies from 42.7 in East Africa, up to 4.4 per 100.000 women in West Asia (Middle East); it is also an important cause of death by a malignant tumor in women with 266.000 deaths per year, 87% of which occur in underdeveloped countries.
In Mexico since 2006 Cervical cancer is the second leading cause of cancer death in women. Each year it is estimated an occurrence of 13.960 cases in women, with an incidence of 23.3 cases per 100.000 women. In the year 2014, there were 3.063 new cases of malignant neoplasms of the uterine cervix with an incidence rate of 6.08 per 100.000 inhabitants over the age of 10 years. The distribution of the cases of cancer of the cervix in relation to age, shows an increase from the 35 years, being the group of 50 to 59 years of age who has the highest percentage with about 30% of all cases registered for the year 2014; the average age of presentation of cases of CCU is 49.2 years. The positivity by Human Papilloma Virus for the year 2014 was 1035, the entities that registered the highest rate of positivity were the states of Veracruz, Tabasco and Chiapas with 13.1, 12.5 and 12.1 respectively. The 82.7% of the reported HPV genotypes correspond to other HPV, a 18.81% to HPV16 and a 3.6% to HPV 18, the rest are due to coinfection of these genotypes. In relation to the histological classification, 46% of the CCU registered, correspond to invasive squamous cell carcinoma, a 23% to microinvasive squamous cell carcinoma, a 10% to endocervical adenocarcinoma in situ, a 6% to invasive endocervical adenocarcinoma, the rest are associated with other histologic types. In relation to the classification by clinical stages of detection of the CCU, the 23.27% correspond to carcinoma in situ, the 25.51% to stages, 16.61% to intermediate stages, a 30.8% to late stages and the 3.79% of cases of CCU tumors are not classifiable. (1)
With regard to the cervical cancer mortality rates in the state of Hidalgo, in the year 2000 there were 75 deaths (9.3 x 100.000 women), in 2001 (11.2) 94, 60 in 2002 (7.1), in 2003 79 (8.6), (9.0) 200485 and 200594 (9.6). (2)
Historical context of the screening tests for CCU and HPV
In 1914 Dr. George Nicholas Papanicolaou performs Pap smears to guinea pigs of the menstrual cycle (technical). For 1927 the doctor Aurel Babes (1886-1962) presented his work on the diagnosis of cancer of the cervix using smears, which he published in 1928.
The researcher Hans Peter Hinselmann invents the colposcope, which I use for the first time in December 1924; through the "acetic acid test". Walter Schiller (1887-1960) In 1928 the test of Lugol's iodine (Schiller improved the technique of scraping with the help of sharp curettes to obtain samples from suspicious areas colposcopicamente, allowing the histological analysis, for what can be considered the precursor of the PAP TEST. The German Karl August Bolten (1912-1972) came to this country as a student in 1953 and developed a school of colposcopy. George Papanicolaou continued working and in 1940 the "perfect the technique PAP" (take-fixation-staining-nomenclature). Dr. Harald zur Hausen proposed in 1975, that the human papilloma virus (HPV) was the etiologic agent of cervical cancer. As for the decade of the 1980s when Guissmann Lutz published the first sequences isolated from HPV warts: HPV-6 and HPV-11; used as hybridization probes for the 16 and 18 subsequently. (3)
At present, the tendency of numerous research groups is to evaluate the possibility of using different molecular techniques for the detection of HPV as a tool in the primary screening of cervical cancer and dysplasia. Despite this, it is important that the techniques applied have a great sensitivity and specificity, in addition to a good reproducibility and negative predictive value, to consider and implement them in the optimal way for the detection of HPV in clinical practice.
The evidence of systematic diagnosis of HPV infection can be classified in visual (colposcopy), microscopic (cytology) and molecular techniques (PCR, hybridization, etc.). The colposcopy is a procedure exploratory instrumented to observe the condition of the epithelium, which are based on the identification of abnormal tissue by a whiteout when applying acetic acid or Lugol's solution. (4)
Conventional Cervical Cytology/PAP
A screening test for the early detection of cervical cancer, consists of obtaining cells from the endocervix and Ectocervix, its extended on the slide, the implementation of the Papanicolaou staining technique and the observation of the sample under a microscope to interpret the changes or alterations in the morphology of the cells. The early detection of cervical cancer by cervical cytology (described by George Papanicolaou in 1943) in the past 50 years has reduced mortality from invasive cancer of the cervix at the global level. (5)
It has a is (6) While thesensitivity of cytology has been reported from 32.4 to 90%, and may not be detected high-grade neoplasia or cancer in more than 35%; produces false negatives of 5 to 35%, and pose a defeat to the timely detection because avanzadamente could be diagnosed later. For this screening is highly sensitive and specific it is necessary that the cytological sample contains cells of the ectocervix and endocervix, that these are appropriately extended in the glovebox and secured correctly, in addition to the adequate implementation of the Papanicolaou staining technique and proper interpretation of the cellular morphological changes (7). There are 3 ways to take the cytology, see the following picture: (Figure 1)
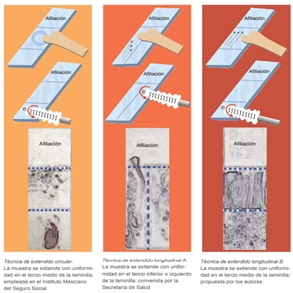
Figure 1. Techniques to extend the ectocervical lesion material.
Source: RAMOS G. Cervical cytology satisfactory, extended ectocervical circular compared with longitudinal. Rev Mex Inst Mex Insurance Soc. 2014; 52(6).
There are criteria for evaluating the quality of the sample, the Bethesda system, incorporated into the Official Mexican Norm NOM-014-SSA2-1994, use the following categories:
• Satisfactory for evaluation (with the specification of whether or not there are elements of the transformation zone).
• Unsatisfactory for evaluation (when the specimen is not identified, the foil is broken or there are factors that impede its interpretation, such as blood or inflammation).
This report sets out the minimum criteria of cellularity and visibility, both glandular as flaky, and stresses the importance of endocervical cells or transformation zone as the primary indicator for the quality of the sample. With this in another range the cellular elements of the exocervix (squamous cell carcinoma), since these are not eligible to decide if the sample is satisfactory for evaluation and refers only to quality indicators, including the minimum cellularity 8000 to 12000 (squamous cell carcinoma) and visibility of the same (minimum 25% of squamous cell overlapping). (8)
Liquid-based Cervical Cytology
Liquid based cytology unlike the conventional extended is not performed in the initial phase, but is transferred the material (sample) to the fixative or preservative, which increases the cytologic detection of squamous intraepithelial lesions and reduce the number of extended unsatisfactory; the sensitivity in liquid base for high-grade intraepithelial lesions (LIEA), low-grade intraepithelial lesions (LIEB) and Atypical cells of undetermined significance (ASCUS), and it was found 57.1%; 79.1% and 90.4%, respectively, with respect to the conventional, with 55.2%, 75.6% and 88.2%, without statistical differences in sensitivity and specificity for cervical neoplasia grade 2, between the conventional technique and the liquid base. (9)
The procedure is to remove the vial the brushes, the liquid is poured into a test tube and centrifuged for 5 minutes 1,500 RPM; excess is removed leaving the sediment, take the brackets for the slides and placed a porta above (identified with a secret code), a filter that has a hole in the center, a kind of funnel and a ring that is turned to hold the other. With an automatic pipette a drop of sediment in the slide through the funnel mentioned before. This support with the slide, the filter and the drop of sediment are placed in a closed container and given 5 minutes of time to 1,500 revolutions per minute. At the end of the centrifugation are removed and disassembled the supports of the packages to be removed from the filter and is fixed; stained each slide with the conventional technique, with hematoxylin-eosin staining as described above for the cytology Pap test and is ready for observation under the microscope, as explained in the following picture (Figure 2). (10)

Figure 2. Process of liquid-based cytology.
Source. Own elaboration, photos taken of Http://www.laboratoriopatologia.com/services-list/radiology/
Visual Inspection with Acetic Acid 5% and Lugol's solution to the 10%
The visual inspection with acetic acid (VIA) implies a direct revision of the cervix under bright light (preferably a halogen bulb lamp) minute after application of a 5% acetic acid diluted acid. This technique is being used as a screening test for cervical cancer in many low- and middle-income countries. The test is simple, feasible and affordable. Allows immediate results for the diagnosis and/or treatment to HIV-positive women. With a sensitivity of 30 to 87% and a specificity of 86-100%. (11)
The acetic acid 5% causes a reversible coagulation or precipitation of the cellular proteins. Also causes swelling of the epithelial tissue, in particular of the columnar epithelium and from any area of the squamous epithelium. It also causes dehydration of the cells and helps to coagulate and clear the mucus in the cervix. The normal squamous epithelium is pink and the columnar epithelium is red, due to the reflection of the light of the underlying stroma highly vascularized. If the epithelium contains a lot of cellular proteins, acetic acid coagulates these proteins that can obscure the color of the stroma. This acetowhite reaction produces a noticeable effect that contrasts with the pinkish color of the surrounding normal squamous epithelium, an effect that is commonly distinguished with the naked eye. The effect of acetic acid depends upon the amount of cellular proteins present in the epithelium. The areas in which there is a nuclear activity and DNA content in high show changes more intense white color. When acetic acid is applied to normal squamous epithelium, little coagulation occurs in the superficial layer of cells, where the nuclei are scarce.
Though the deeper cells contain more nuclear protein, the acetic acid does not penetrate sufficiently and, hence, the resulting precipitation does not overshadow the color of the underlying stroma. The CIN and invasive cancer undergo maximal coagulation due to their higher content of nuclear protein (in view of the large number of undifferentiated cells contained in the epithelium) and prevent light from passing through the epithelium. As a result, the subepithelial vascular pattern is hidden and the epithelium takes a dense white color. In the event of a NIC, the acetowhitening is restricted to the transformation zone close to the squamocolumnar junction, while in the case of a cancer, this reaction often involves the entire cervix, as shown in the Figure 3. (12)
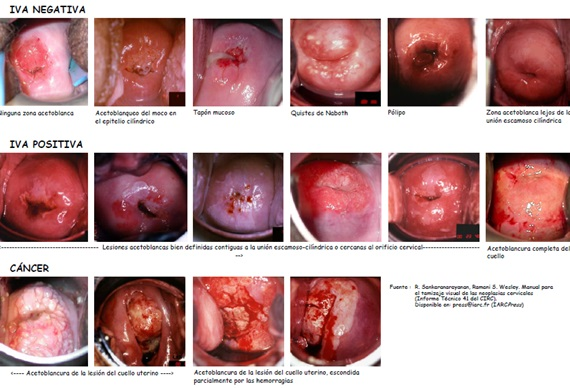
Figure 3. Clinical Reference Chart for visual inspection after application of acetic acid.
Source: R. Sankaranarayanan, Ramani S. Wesley. Manual for the screening of cervical neoplasia (Technical Report 41)
The inspection with Lugol's solution to the 10% is a direct screening test which has a sensitivity of 87.2% and a specificity of 84.7%. The metaplastic squamous epithelium contains glycogen while CIN and invasive cancer contain little or no glycogen.
The columnar epithelium does not contain glycogen, as well as the immature squamous metaplastic epithelium or, occasionally, you can hold it in low amounts. For its part, the iodine is glucofilico and, consequently, the application of an iodine solution gives rise to the iodine uptake by the epithelia that contain glycogen.
Thus, the normal squamous epithelium, which if it contains glycogen, stained mahogany brown or black after the lugolizacion. In contrast, the columnar epithelium does not capture the iodine and not stained, and even may appear slightly discolored due to a thin layer of Lugol's solution. Similarly, the areas of immature squamous metaplastic epithelium may not stain with iodine or dye in a partial way. If there is scaling (or erosion) of superficial and intermediate cell layers as a result of inflammatory conditions of the squamous epithelium, these areas do not stain with iodine and remain colorless clearly against a black background, or mahogany. Areas of CIN and invasive cancer do not take up iodine (as they lack glycogen) and appear as thick mustard yellow or saffron. Areas with leukoplakia (hyperkeratosis) do not stain with iodine. As for the condylomas can, at times, partially stained with iodine, as can be seen in the Figure 4. (13)
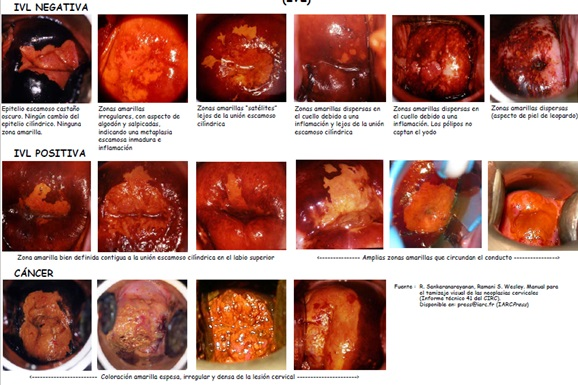
Figure 4. Clinical Reference Chart for Visual Inspection after applying the yodoyodurada of Lugol's solution.
Source: R. Sankaranarayanan, Ramani S. Wesley. Manual for the screening of cervical neoplasia (Technical Report 41).
Cervical Colposcopy
The colposcopy is a procedure by which displays the epithelium and the plot sub epithelial cancer of the cervix, a colposcope with amplifications from 7.5 X 30, 15X and X, contributes to the diagnosis, location, extent of injury and histologic features intraepithelial lesions. With a sensitivity of 83% of the colposcopy and specificity of 86%. (14)
The colposcopy is the gold standard to diagnose and guide the treatment of high-grade cervical neoplasia, but on the other hand, malfunctioning, without standards in education, training and practice of colposcopy. (15)
The colposcopy should be done only when lesions are present for cytological confirmation or reaction of polymerase chain reaction. The colposcopic findings may vary depending on the types of HPV. In particular, work-related injuries the type 16 are more definitive and larger than other types. (16)
Hybrid Capture II and III
The monocatenario nucleic acid molecules that are complementary to form hybrids in appropriate conditions. The evidence of hybridization are based on this phenomenon and used marked probe molecules to detect specific complementary target molecules.
The nucleic acid hybridization III is the most sensitive method to detect HPV in clinical samples, and the only one able to identify specific types of HPV, detects the DNA of 14 high-risk types of HPV genotype HPV16 / 18 (17); While hybridization II HC2 allows the detection of 13 HPV genotypes (HPV 16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59 and 68) by hybridization with probes of RNA and amplification of the signal. (18) The hybridization III has a sensitivity of 87.7% to 96.9% and specificity of 90.6% to 91.7% (18); while the hybridization II has a sensitivity of 96% and specificity of 66.7%. (19)
The procedure involves taking a sample with cervical brush which is placed in the road; the samples were denatured manually before the analysis of hybridization II in the rapid capture automated or manually. Hybridized with viral particles and the detection and reading; as can be seen in the Figure 5.
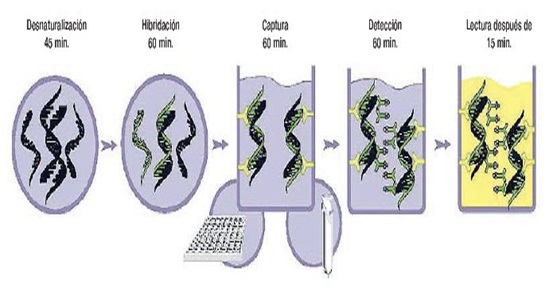
Figure 5. Process of hybridization.
Source: Obtained from http://www.inmunolab.com/attachments/38/LBcaptura_hibrida___qiagen.pdf
Polymerase Chain Reaction
Amplification of the viral genome by PCR method to discriminate the type of HPV, able to detect between 10 and 200 copies of the viral genome per sample. Detect the target DNA by using oligonucleotide primers that complement in a specific way with the flanking regions of DNA to amplify gene L1. The state of latency affects the sensitivity of the PCR, especially if the sample was taken from an area where the carriers are scarce or absent. (20) This may explain why samples negative by PCR. (21) Has demonstrated better sensitivity (between 83.9% and 100%) that the cytology for the detection of HPV, but with a lower specificity (64.1% to 95.1%). (22)
The sample is taken with endocervical swab, the sample is placed in a viral way, using primers directed against the high risk human papilloma virus (16, 18 is reported and high-risk (total 27); viral DNA is extracted and purified; there is a polymerase chain reaction with the DNA extracted, (23) They were separated and detected in terms of their size through the use of capillary electrophoresis. (24)
The high-risk viruses are high risk (26, 31, 33, 35, 39, 45, 51, 52.53, 56, 58, 59, 66, 68, 73, 82). (25)
Conclusions
Throughout the history of cervical cancer screening, tools have been created and perfected for the timely detection of human papillomavirus, cervical lesions and Cervical cancer; according to this review we can say that for the detection of human papillomavirus the best tool today is PCR due to its high sensitivity and specificity (cost-benefit); as well as allowing a greater number of detected viruses, as can be seen in table number 1, currently in Mexico this tool is applied instead of hybridization that only allowed to detect or not the infection without genotyping it, the first one in combination with liquid based cytology which decreases the incidence of poor fixation and therefore poor diagnostic reading; Regarding the detection of cervical lesions, the best tool is liquid based cytology since it provides a greater sensitivity and specificity compared to the conventional one, which requires constant training by the staff for a correct fixation or spread in the lamilla, the which is the error number 1 for the lack of cellularity to its reading and with this negative results can be given, nevertheless the European union according to the made revisions determined that the GOLD STANDARD is the colposcopy; however, it is less sensitive and specific with 83% and 84% compared to conventional or liquid cytology, emphasizing that it is an exploratory study which allows visual inspection with acetic acid or Lugol, as well as biopsy and even treatment. , provided it is performed before a positive screening to cervical lesion; As for the inspection with acetic acid and Lugol are good tools with good sensitivity and specificity but allow a late detection since the process of malignization would be advanced before positive tests, derived that its positivity is according to the amount of proteins present (acetic) ) in lesions or carcinoma and presence of glycogen (Lugol), but its low cost and reproducibility makes it an accessible study for low-income countries.
Given this, each country will take the most appropriate tool for its screening since not all of them are accessible and depend on the economy of the country; likewise of his priorities in public health.
Recommending from a scientific point the tests of liquid based cytology, PCR (polymerase chain reaction) and colposcopy; for the correct and timely detection of cervical cancer and human papillomavirus; with a high sensitivity and specificity.
This review article allows the reader to deepen their knowledge in Cervical Cancer Screening and in the same way make criticisms and test these screening tools.
Negative aspects
With the previous review it is inferred that the use of screening tests such as conventional cytology, inspection with acetic acid or Lugol derived from its sensitivity and specificity that can lead to false positives in the diagnoses is negative or erroneous; this in terms of cervical injuries or cervical cancer. Regarding the genotypic detection of the papilloma virus, the use of hybridization is not correct since it has a low range for virus identification, as the first tests only allow to discriminate between high and low risk of the virus making it a test with low cost-benefit level (Table 1).
|
Table 1. Summary of screening tests for cervical cancer and human papillomavirus |
||||
|
Test |
Detects |
Use |
Sensitivity |
Specificity |
|
Conventional cytology / Pap |
Abnormal cells |
Possible cervical lesions |
32.4 to 90% |
94% |
|
Liquid-based cytology |
Abnormal cells |
Possible cervical lesions |
79.1% to 90.4% |
NA |
|
Visual inspection of the acetic acid |
Cervical lesions visible |
Possible cervical lesions |
30 to 87% |
86 to 100% |
|
Visual inspection Lugol |
Cervical lesions visible |
Possible cervical lesions |
87.2% |
84.7%. |
|
Colposcopy |
Cervical Neoplasia |
Cervical lesions |
83% |
86% |
|
Hybrid II |
Hpv |
Hpv detection of high and low risk (13 types) |
96% |
66.7% |
|
Hybrid III |
Hpv |
Hpv detection of high and low risk (13 types) |
87.7 to 96.9% |
90.6% |
|
PCR |
Hpv |
Hpv detection of high and low risk (27 types) |
83.9 to 100% |
64.1 to 95.1% |
Source: own elaboration, data obtained from the references consulted.
References
|
1. |
Secretaria de Salud. Programa de Accion Especifico Prevencion y Control del Cancer de la Mujer 2013-2018. Programa. Mexico: Secretaria de Salud. |
|
2. |
Olvera M. Prevalencia de cáncer cérvico uterino, lesiones premalignas y. Gaceta Hidalguense de Investigación en Salud. 2015; 8(2). |
|
3. |
Herrera Y. Historia de la evolucion de las pruebas de tamizaje de cancer cervicouterino. Rev Med Inst Mex Seguro Soc. 2015; 53(6). |
|
4. |
Gutierrez R. Utilidad de las tecnicas moleculares de deteccion de VPH en el control y prevecion del cancer cervicouterino. AMATGI. 2011; III(5). |
|
5. |
Ramos G. Citologia cervical satisfactoria, extendido exocervical circular comparado con longitudinal. Rev Mex Inst Mex Seguro Soc. 2014; 52(6). |
|
6. |
Carrascal M. Correlacion diagnostica de la citologia cervical versus colposcopia en lesiones premalignas de cancer cervicouterino. IPS Universitaria Barranquilla. 2013; 9(1). |
|
7. |
Sanchez M. Certeza diagnostica de la colposcopia, citologia e histologia de las lesiones intraepiteliales del cervix. Rev Invest Med Sur Mex. 2013; 20(2). |
|
8. |
Secretaria de Salud. Modificacion a la Norma Oficial Mexicana NOM-014-SSA2-1994, para la prevencion, deteccion, diagnostico, tratamiento, control y vigilancia epidemiologica del cancer cervicouterino. Norma Oficial Mexicana. Mexico : Secretaria de Salud. |
|
9. |
Contreras R. Papanicolaou y citologia liquida en diagnostico de cancer de cervix. Hospital civil de Maracay. Comunidad y Salud. 2015; 13(1). |
|
10. |
Puerto de Amaya M. Citologia convencional y en base liquida en muestra compartida de tomas cervicouterinas. Repert Med Cir. 2015; 24(1). |
|
11. |
Mittal S. Visual inspection with acetic as a screening test for cervical cancer. Biomed Res. 2013; 1(1). |
|
12. |
R S. Análisis y registro de los resultados de la inspección visual con ácido acético al 5% (IVA). En R S. Manual practico para la deteccion visual de las neoplasias cervical. Lyon, Francia; 2005. p. 50. |
|
13. |
Sankaranarayanan R. Early detection of cervical cancer with visual inspection methods: a summary of completed and on-going studies in India. Salud Publica Mex. 2003; 45(3). |
|
14. |
Gonzalez G. Grado de efectividad y correlacion citologia-colposcopia utilizadas como pruebas diagnosticas en una entidad de salud de Santa Marta. DUAZARY. 2013; 10(2). |
|
15. |
Ulrich K. 2017 update of the European Federation for Colposcopy (EFC) performance standards fot the practice of colposcopy. European Journal of Obstetrics & Gynecology and Reprouctive Biology. 2018; 224. |
|
16. |
Nam K. Colposcopy at a turning point. Obstet Gynecol Sci. 2018; 61(1). |
|
17. |
Zhao X. The performance of human papillomavirus DNA detection with type 16/18 genotyping by hybrid capture in primary test of cervical cancer screening: a cross-sectional study in 10.669 Chinese women. Clinical Microbiology and Infection xxx. 2018. |
|
18. |
Lactobellis M. Clinical validation of Realquality RQ-HPV screen according to the international guidelines for human papillomavirus DNA test requirements for cervical screening. Virology Journal. 2018; 15(48). |
|
19. |
Gutierrez L. Molecular diagnosis of human papillomavirus in the development of cervical cancer. Salud publica de Mexico. 2009; 51. |
|
20. |
Moller D. Clinical and analytical performance of the BD Onclarity HPV assay for detection of CIN2 lesiones on SurePath samples. Papillomavirus Research. ; 2. |
|
21. |
Astudillo O. Diagnostico molecular del virus del papiloma humano. Panoram Medico. 2014; 8(1). |
|
22. |
Sanoja L. Deteccion y tipificacion del virus del papiloma humano mediante reaccion en cadena de polimerasa, en muestras cervicales de estudiantes. Comunidad y Salud. 2013; 11(2). |
|
23. |
Sharafadeen K. Prevalence and risk factors for genital hish-risk human papillomavirus infection among women attendin the outpatient clinics of a university teaching hospital in Lagos, Nigeria. Pan African Medical Journal. 2017; 28. |
|
24. |
Beyazit F. The prevalence of human papillomavirus (HPV) genotypes detected by PCR in women tih normal and abnormal cervico-vaginal cytology. Comunidad y Salud. 2018; 11(2). |
|
25. |
Aleksioska I. Prevalence of specific types of human papiloma virus in cervical intraepithelial lesions and cervical cancer in Macedonianan women. Med Arch. 2018; 71(1). |
